What is Gabapentin?
Gabapentin, a synthetic analog of the neurotransmitter gamma-aminobutyric acid (GABA), is primarily utilized in the clinical management of neurological conditions. Initially approved by the U.S. Food and Drug Administration (FDA) in 1993 for the treatment of epilepsy, Gabapentin has since garnered attention for its efficacy in addressing neuropathic pain, postherpetic neuralgia, and various off-label uses, including anxiety disorders and restless leg syndrome.
The primary mechanism of action of Gabapentin involves the modulation of calcium channels in the nervous system. By binding to the alpha-2-delta subunit of voltage-gated calcium channels, Gabapentin inhibits the influx of calcium ions, thereby reducing the release of excitatory neurotransmitters. This modulation helps alleviate neuronal hyperexcitability, which is a characteristic feature of epilepsy and neuropathic pain syndromes. As a result, Gabapentin is often recommended as part of a multimodal approach to pain management, particularly for conditions resistant to over-the-counter analgesics.
Its therapeutic applications extend beyond epilepsy and neuropathic pain. Clinicians increasingly prescribe Gabapentin for conditions involving anxiety and mood disorders, as it can produce anxiolytic effects without the addictive potential associated with benzodiazepines. Though further research is required to solidify these applications, the drug is often integrated into treatment regimens aimed at addressing comorbid psychiatric disorders in patients suffering from chronic pain.
The pharmacokinetics of Gabapentin are noteworthy, as it has a relatively low bioavailability that decreases with increasing doses, necessitating careful titration when initiating therapy. Patients often experience dose-dependent side effects, which may include dizziness, fatigue, and somnolence. Despite its generally favorable safety profile, the potential for misuse and dependence, particularly in populations with a history of substance abuse, has raised concerns in clinical practice.
In recent years, the discussion surrounding Gabapentin has evolved, with emerging evidence pointing to its potential interaction with the opioid epidemic. Prescribing Gabapentin alongside opioids may pose a risk of enhanced central nervous system depression, necessitating cautious prescribing practices and vigilant monitoring.
How Does Gabapentin Affect the Brain?
Gabapentin, a medication originally developed for the treatment of epilepsy, has gained widespread use in the management of neuropathic pain and as an adjunct therapy for certain anxiety disorders. While its clinical applications continue to expand, an understanding of its neuropharmacology reveals significant insights into how it interacts with the brain’s biochemical pathways.
Structurally related to the neurotransmitter gamma-aminobutyric acid (GABA), gabapentin does not bind directly to GABA receptors, which differentiates it from traditional anxiolytic medications that utilize GABAergic pathways. Instead, gabapentin exerts its effects primarily through its interaction with the alpha-2-delta subunit of voltage-gated calcium channels in the central nervous system. By binding to these channels, gabapentin modulates the influx of calcium ions into neurons, subsequently reducing the release of several excitatory neurotransmitters, including substance P, glutamate, and norepinephrine. This action leads to a decrease in neuronal excitability and ultimately results in the alleviation of pain and seizure activity.
Clinical evidence suggests that gabapentin’s mechanism also extends to its potential anxiolytic properties. By inhibiting excessive neuronal firing and stabilizing synaptic transmission, gabapentin can mitigate the heightened synaptic activity often observed in anxiety disorders. This property is particularly relevant in conditions characterized by hyperarousal and heightened reactivity, where gabapentin may help to restore a more balanced state.
Furthermore, gabapentin’s influence on the brain’s neurotransmitter systems suggests promising avenues for treating various psychiatric disorders. The reduction of excitatory neurotransmitter release may explain its utility in conditions such as generalized anxiety disorder and post-traumatic stress disorder. However, while gabapentin shows efficacy in these realms, it is imperative to approach its use with caution, as it is associated with a range of side effects including sedation, dizziness, and in some cases, potential dependency.
In addition, ongoing research into gabapentin highlights the importance of understanding individual variability in response to the medication. Genetic differences affecting drug metabolism, receptor sensitivity, and neurological condition predispositions might all influence treatment outcomes. Ultimately, while gabapentin represents a crucial therapeutic option within neurology and psychiatry, its brain effects underscore a need for further research to fully elucidate its long-term implications and to optimize its application in clinical practice. As our understanding of gabapentin deepens, it becomes increasingly clear that its multifaceted interactions with the central nervous system warrant careful consideration within a comprehensive treatment framework.
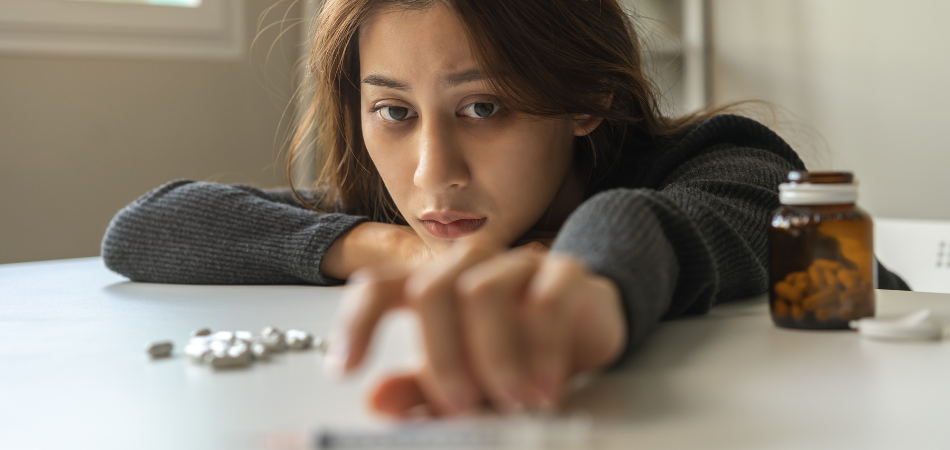
How and Why is Gabapentin Abused?
Gabapentin, a medication primarily prescribed for epilepsy and neuropathic pain, has garnered attention in recent years due to its increasing misuse and abuse. Originally developed to aid individuals suffering from seizures, its off-label applications for anxiety and chronic pain management have contributed to a surge in prescriptions. However, the sedative effects that some users experience have led to its misuse, raising concerns about the potential for addiction and dependence.
One significant factor contributing to the abuse of gabapentin is its perception as a “safer” alternative to traditional opioids. In the backdrop of an opioid crisis that has devastated countless lives, gabapentin is often viewed as a non-opioid option for pain relief, leading some individuals to self-medicate without proper guidance from healthcare professionals. As individuals seek to alleviate discomfort or emotional distress, they may inadvertently escalate their usage, unaware of the risks associated with misuse.
The mechanism of gabapentin’s action also plays a role in its abuse potential. While it is not classified as a controlled substance, at high doses, gabapentin can produce effects akin to euphoria or relaxation, particularly when combined with other depressants such as opioids or alcohol. Users may become accustomed to these effects, leading them to increase their dosage to achieve the desired sensations. This cycle of escalating use can result in tolerance, dependence, and withdrawal symptoms, fostering a compulsive pattern of behavior surrounding the substance.
Furthermore, the social stigma around gabapentin is less pronounced than that of stronger narcotics, which may encourage individuals to misuse it with a lower perceived risk of damaging their reputation or facing legal consequences. The absence of rigorous monitoring and regulation surrounding gabapentin prescriptions further exacerbates the issue, as patients can often acquire the drug without sufficient medical oversight. Toxicological studies indicate a troubling correlation between increased gabapentin prescriptions and rising rates of misuse, signaling an urgent need for increased awareness and education about the risks.
The abuse of gabapentin is a complex phenomenon driven by its perceived safety, sedative effects, and societal attitudes towards prescription medications. As healthcare practitioners strive to provide effective pain management, caution must be exercised to prevent the emergence of dependence and misuse of this once-respected pharmaceutical agent. Enhanced education for both prescribers and patients, alongside closer monitoring and regulation, is crucial in mitigating the risks associated with gabapentin abuse and safeguarding public health.
Is Gabapentin Addictive?
Gabapentin, a medication initially designed to treat epilepsy and neuropathic pain, has gained notoriety in contemporary discussions regarding prescription drug use and potential addiction. With the alarming rise in the misuse of various pharmaceuticals, particularly opioids, it is imperative to scrutinize the properties of gabapentin to determine whether it possesses addictive qualities. The following will explore the pharmacological profile of gabapentin, its potential for abuse, the scientific literature surrounding its addictive properties, and the implications for medical practice and patient care.
Gabapentin, chemically known as 2-(1(aminomethyl)cyclohexyl)butanoic acid, was approved by the United States Food and Drug Administration (FDA) in 1993. The drug works primarily by modulating synaptic transmission in the central nervous system, particularly by inhibiting the release of excitatory neurotransmitters. Its principal indications include the treatment of neuropathic pain and as an adjunctive therapy in treating seizures. Despite these medical applications, the question of whether gabapentin carries a risk of addiction deserves further exploration.
Understanding addiction necessitates a comprehensive examination of the characteristics that typically define addictive substances. The National Institute on Drug Abuse (NIDA) outlines several criteria for a substance to be considered addictive, including reinforcing effects, withdrawal symptoms, and compulsive use despite harmful consequences. When evaluating gabapentin against these standards, its profile appears notably different from that of more commonly abused substances, such as opioids, benzodiazepines, or stimulants.
First and foremost, gabapentin lacks the reinforcing effects associated with addictive drugs. Research indicates that gabapentin does not produce the euphoric high often sought by individuals who misuse substances. Studies examining animal models of addiction consistently report that gabapentin does not elevate dopamine levels in the brain’s reward pathways—an effect that is central to the reinforcing properties of more addictive drugs. Consequently, the absence of a euphoric effect contributes to gabapentin’s lower potential for abuse.
Additionally, research highlights that gabapentin is not generally associated with withdrawal symptoms upon cessation, a characteristic often seen in addictive substances. While some users may report minor discomfort upon discontinuation, these symptoms do not approach the severity or complexity experienced with drugs like opioids or alcohol. Nonetheless, it is critical to recognize that abrupt cessation can lead to the recurrence of the underlying condition for which gabapentin was prescribed, complicating the clinical picture further.
Despite the evidence suggesting a lower potential for addiction, the increasing prescription of gabapentin has raised concerns among healthcare professionals and regulatory bodies. The drug is sometimes prescribed off-label for conditions such as anxiety and insomnia, which do not fall within its established indications. This off-label use has led to a burgeoning interest in its potential for misuse, particularly in individuals with a history of substance abuse disorders. Several studies have indicated that gabapentin can enhance the effects of opioids and other central nervous system depressants, leading to recommendations for caution when prescribing it in conjunction with these medications.
In light of the aforementioned factors, it is essential to recognize that while gabapentin does not exhibit the classic characteristics of an addictive substance, it is still capable of misuse in specific contexts. Reports of individuals seeking gabapentin prescriptions for recreational purposes have been documented. Additionally, there is a small but notable subset of patients—particularly those with co-occurring substance use disorders—who may engage in compulsive use. Therefore, although the risk of gabapentin addiction is significantly lower than that of other substances, vigilance is warranted.

Treatment at TRUE for Gabapentin Addiction
Gabapentin, initially developed for the treatment of epilepsy, has increasingly gained prominence as a substance associated with addiction and dependency. While it is prescribed for neuropathic pain and anxiety disorders, misuse of gabapentin has emerged as a significant public health concern. Individuals may develop a tolerance, leading them to increase dosages beyond what is medically advisable, thus necessitating specialized treatment pathways. TRUE Addiction and Behavioral Health offers a structured environment tailored for those grappling with gabapentin addiction, focusing on evidence-based methodologies that foster recovery.
The treatment model at TRUE Addiction and Behavioral Health emphasizes a holistic approach to addiction recovery. The initial stage involves comprehensive assessments, including medical history evaluations and psychological screenings. This ensures that clinicians are equipped with an accurate understanding of an individual’s specific needs, which is critical for tailoring an effective treatment plan. Recognizing that gabapentin addiction often co-occurs with other mental health disorders such as anxiety or depression, TRUE’s multidisciplinary team is trained to address these overlapping issues concurrently, enhancing the overall likelihood of successful recovery.
Throughout the treatment process, TRUE Addiction and Behavioral Health employs a combination of pharmacological and therapeutic interventions. While detoxification may be necessary to manage withdrawal symptoms safely, the facility’s focus extends beyond mere cessation of use. Utilizing cognitive-behavioral therapy (CBT) and motivational interviewing, therapists guide patients in identifying the underlying psychological triggers of their substance use. This promotes self-awareness, equipping individuals with the skills to respond to cravings and stressors in healthier ways.
Furthermore, TRUE Addiction and Behavioral Health prioritizes aftercare and relapse prevention strategies. Recognizing that recovery from gabapentin addiction is an ongoing journey, the organization offers continued support through outpatient programs and group therapy sessions. These initiatives foster a sense of community among participants, which can be vital in maintaining sobriety. Peer interactions enable individuals to share experiences and strategies, thus reinforcing their commitment to a drug-free lifestyle.
TRUE Addiction and Behavioral Health represents a commendable facility committed to addressing the complexities of gabapentin addiction. Through a comprehensive and individualized treatment plan that integrates medical, therapeutic, and social support, the organization stands as a beacon of hope for those seeking recovery. By addressing both the physiological and psychological aspects of addiction, TRUE Addiction and Behavioral Health provides a robust framework that enhances the prospects of lasting recovery and improved quality of life for individuals impacted by gabapentin misuse.
In Conclusion
In conclusion, gabapentin is primarily categorized as a non-addictive medication based on its pharmacological properties and the absence of traditional addiction criteria, but it is in fact addictive. However, as prescribing practices evolve and off-label uses expand, healthcare professionals must remain alert to the potential for misuse, particularly among vulnerable populations. Accurate patient assessment, monitoring, and education regarding the proper use of gabapentin are vital components of responsible prescribing.
If you or someone you know is struggling with substance abuse or a mental health issue, contact TRUE today to get started on the path to long-term successful recovery. TRUE is a premier provider of addiction and mental health services located in Tennessee. TRUE offers the most comprehensive menu of services for people in need of Tennessee mental health treatment and for those struggling with substance use disorder.
Verify Your Insurance Online
We are here to help. Contact us today and get the answers you need to start your journey to recovery!
